Meniere’s Disease
How is it that Dr Sutter, a dentist, can treat and improve the symptoms of Meniere’s Disease (MD)?
That is a great question. I had someone close to me mention “My Meniere’s is really acting up today.” This was a disease I was ignorant of, so I went and looked up symptoms along with treatments. The symptoms sounded very familiar and paralleled many of the TMD symptoms that I am very familiar with. I gave the patient a signs and symptoms questionnaire and asked her to circle all of her symptoms. I wanted to see if those were the only symptoms she had.
As it turned out she had those MD symptoms as well as symptoms of TMD that she had never mentioned them before. She had reported having audiology tests and was diagnosed with MD by an Ear, Nose and Throat doctor. Not by me. I ran a series of test on her to see if there was an underlying dental cause for the symptoms she had. She reported fullness of the ear, tinnitus, and periods of decreased hearing loss as well as periods where she was super sensitive to sound. All of these symptoms occurred on the left side. There were also the transient periods of vertigo as well. The tests were run and she demonstrated elevated surface EMG resting electrical activity levels in the left temporalis muscle (Fig. 1).
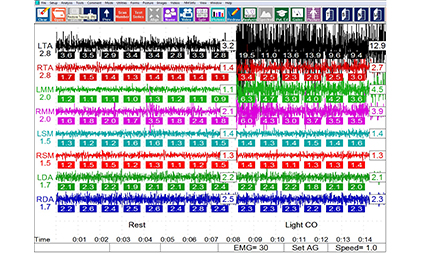
Figure 1. EMG data of the right and left anterior temporalis (LTA, RTA), the bilateral masseter (LMM, RMM), sternocleidomastoid (LSM, RSM) and anterior digastric (LDA, RDA) muscles. The left pane shows asymptomatic average patient reference microvolts, whereas the numbers at the bottom of each EMG reading are unique to the individual patient being measured. The left half of the scan is the resting muscle activity (no tooth contact) while the right half illustrates the muscle output when during light occlusal contact in Centric Occlusion (MIP). Note the left masseter Muscle (LMM) shows more than four and a half times the output of the right masseter muscle (12.9 microvolts, 2.7 microvolts respectively) when teeth are in light occlusal contact, indicating functional asymmetry with left masseter hyperactivity.
Maximum opening exceeded 50 mm, with a restricted range of motion in the left excursion of 5.7 mm (Fig. 2). T-Scan occlusal analysis showed a pre-treatment occlusal force imbalance of 56.9% left to 43.1% right, with 47.9% of the total occlusal force present on the left side molar teeth (Fig. 3). Left excursive pretreatment Disclusion Time were longer on the left than the right. The measured diagnostics of occlusal force distribution, prolonged Disclusion Time durations, elevated muscle contraction levels, and the reduced left excursive range of motion, all together indicated that functional problems existed with the left side dentition.
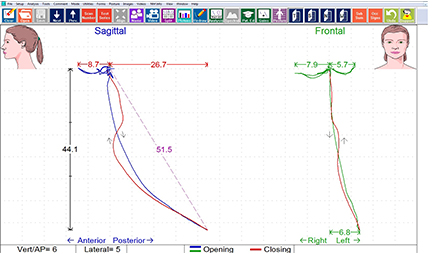
Figure 2. K7 mandibular tracking scan where the frontal view describes a 6.8mm deviation to the left upon opening, and a more restricted left lateral movement compared to the right (5.7 mm left vs. 7.9 mm right).
This correlated well to the left ear being affected symptomatically with stuffiness and tinnitus. We treated the disclusion times and bite force discrepancies (the underlying dental concerns) and her symptoms diagnosed as MD went away. So either it was a misdiagnosis or MD is a subset of TMD. Either way TMD treatments have been shown to improve MD symptoms as reported in the literature (see below).
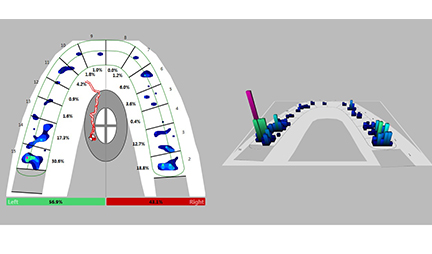
Figure 3. T-Scan 8 2D and 3D occlusal force distribution illustrating that pre-DTR, a 56.9% left to 43.1% right occlusal force imbalance existed, with 47.9% of the total occlusal force concentrated on the left molar teeth.
This scenario has played out a few different times and now people with a diagnosis of MD that are wanting my set of diagnostic tests completed to see if there is an undiagnosed dental reason for the symptoms.
Are the symptoms of TMD and Meniere’s Disease really that similar?
Yes! Very similar. You can check out various websites including www.menieresfoundation.org and see that vertigo, hearing loss and sensitivity to loud sounds, tinnitus and a fullness in the ear are all symptoms of MD…and TMD. Click here and see if you have other symptoms that might suggest problems resulting from a bad bite.
Is Dr. Sutter the only doctor that has made a MD and TMD connection?
Absolutely not. The following articles published show a link between MD and TMD. Interestingly a literature search at NCBI’s PubMed failed to generate a single publication that refuted these observations.
- Bjorne A, Agerberg G. Symptom relief after treatment of temporomandibular and cervical spine disorders in patients with Meniere's disease: a three-year follow-up. Cranio. 2003 Jan;21(1):50-60. (Read Abstract below)
- Bjorne A, Agerberg G. Reduction in sick leave and costs to society of patients with Meniere's disease after treatment of temporomandibular and cervical spine disorders: a controlled six-year cost-benefit study. Cranio. 2003 Apr;21(2):136-43. (Read Abstract below)
- Bjorne A, Berven A, Agerberg G Cervical signs and symptoms in patients with Meniere's disease: a controlled study. Cranio. 1998 Jul;16(3):194-202. (Read Abstract below)
- Bjorne A, Agerberg G. Craniomandibular disorders in patients with Menière's disease: a controlled study. J Orofac Pain. 1996 Winter;10(1):28-37. (Read Abstract below)
- Kempf HG1, Roller R, Mühlbradt L. Correlation between inner ear disorders and temporomandibular joint diseases. HNO. 1993 Jan;41(1):7-10. [Article in German] (Read Abstract below)
- Franz B, Anderson C. The potential role of joint injury and eustachian tube dysfunction in the genesis of secondary Ménière's disease. Int Tinnitus J. 2007;13(2):132-7. (Read Abstract below)
- Björne A. Assessment of temporomandibular and cervical spine disorders in tinnitus patients. Prog Brain Res. 2007;166:215-9. (Read Abstract below)
- Sutter, B. Two case reports of Meniere’s Disease that responded to computer-guided occlusal therapy. International College of Cranio-Mandibular Orthopedics Anthology 2016 in press. (Read Abstract below)
So, Dr. Sutter does treat Meniere’s Disease?
Yes and No. It is not unusual for people that have been diagnosed with Meniere’s to seek out our office. Regardless of any previous diagnosis, we have a protocol that examines muscles, joints, and the bite. If there is an underlying dental concern (bite force or timing discrepancy) we treat the dental anomalies. If after a comprehensive exam, imaging, and diagnostics there is no dental justification consistent with symptoms, we do not proceed with therapy of any kind.
Is it really possible I could have been misdiagnosed?
Yes it is, and it is unfortunate. It is not anyone’s fault, but different specialties look at different things. This is best illustrated with the lesson of “The Blind Men and the Elephant." The lesson is designed to teach that perspective is not always truth. Medicine tends to be very compartmentalized and dentistry is no different. It is easy to imagine different specialties looking at their part of the elephant and thinking it is one thing versus another.
TMD is a great imposter disease and can look like many different things. According to the Mayo Clinic a diagnosis of Meniere’s Disease includes an exam and a medical history by your physician and requires two episodes of vertigo, each lasting 20 minutes or longer but not longer than 24 hours, hearing loss verified by a hearing test, tinnitus or a feeling of fullness in your ear AND exclusion of other known causes of these problems. This last requirement is where things tend to fall short a bit.
Symptom relief after treatment of temporomandibular and cervical spine disorders in patients with Meniere's disease: a three-year follow-up.
Bjorne A, Agerberg G.
Abstract
This study describes the coordinated treatment of temporomandibular disorders (TMD) and cervical spine disorders in patients diagnosed with Meniere's disease. The aim was to follow up treatment outcomes for three years with regular follow-up examinations every six months. Of the 31 patients with Meniere's disease who participated in a controlled comparative study on the signs and symptoms of TMD, 24 participated in a subsequent controlled comparative study on the signs and symptoms of cervical spine disorders (CSD). These 24 Meniere's disease patients (ten males and 14 females) agreed to participate in this longitudinal study. At each follow-up, their symptoms were evaluated using self-administered questionnaires and visual analog scales (VAS). The results of the coordinated treatment showed simultaneous decreases in the intensities of vertigo, nonwhirling dizziness, tinnitus, feeling of fullness in the ear, pain in the face and jaws, pain in the neck and shoulders, and headache that were both longitudinal and highly significant. Significant longitudinal reductions in the frequencies of vertigo, nonwhirling dizziness, and headache were also reported by the patients as well as a complete disappearance of pain located in the vertex area. A significant relief of TMD symptoms and a decrease in nervousness was also achieved. The results showed that a coordinated treatment of TMD and CSD in patients with Meniere's disease is an effective therapy for symptoms of this disease. The results also suggested that Meniere's disease has a clear association with TMD and CSD and that these three ailments appeared to be caused by the same stress, nervousness, and muscular tension.
Cranio. 2003 Apr;21(2):136-43.
Reduction in sick leave and costs to society of patients with Meniere's disease after treatment of temporomandibular and cervical spine disorders: a controlled six-year cost-benefit study.
Bjorne A, Agerberg G<.
Abstract
This study compares the frequency of sick leave between the three-year period after and the three-year period before coordinated treatment of temporomandibular and cervical spine disorders in 24 patients (ten males and 14 females) diagnosed with Meniere's disease. The frequency of sick leave for the patients was also compared with the frequency of sick leave in a control group from the population. A cost-benefit analysis was made regarding the costs to society of sick leave related to the treatment costs of the patients. In a previous study the same patients were treated for their severe signs and symptoms of temporomandibular and cervical spine disorders, and they reported a substantial reduction in their vertigo, non-whirling dizziness, tinnitus, feeling of fullness in the ear, pain in the face and jaws, pain in the neck and shoulders, and headache. The number of days of sick leave and the year the patient began to receive disability pension due to the symptoms of Meniere's disease were obtained from the National Health Insurance Service in Sweden. Two of the patients received disability pension benefits due to Meniere's disease 17 years prior to their normal retirement pension. A third patient received disability pension for another reason and two were receiving a retirement pension. Data on the remaining 19 patients showed a considerable reduction in number of days of sick leave during the three-year period after coordinated treatment (270 days) compared with the three-year period before the treatment (1,536 days). The control subjects used a total of 14 days sick leave for the same symptoms during the same six-year period. Vertigo (nine days) was the dominant cause followed by pain in the neck and shoulders, and headache. The reduction in sick leave for the 19 nonretired patients and the treatment costs for the 24 patients can be used for a simple cost-benefit calculation for the subgroup of nonretired patients. During the first three years after treatment the reduction in sick leave was on average 66.6 days for each of the 19 nonretired patients. Within the limits of this study, it can be concluded that the costs to society for sick leave and disability pension due to Meniere's disease are substantial. A coordinated treatment of temporomandibular and cervical spine disorders appears to substantially reduce these costs.
Cranio. 1998 Jul;16(3):194-202.
Cervical signs and symptoms in patients with Meniere's disease: a controlled study.
Bjorne A, Berven A, Agerberg G.
Abstract
This study compares the frequency of signs and symptoms from the cervical spine in 24 patients diagnosed with Meniere's disease and 24 control subjects from a population sample. From a previous controlled comparative study concerning signs and symptoms of craniomandibular disorders, 24 patients diagnosed with Meniere's disease (10 males and 14 females) and their 24 matched control subjects participated in this investigation on the state of the cervical spine. Symptoms of cervical spine disorders, such as head and neck/shoulder pain, were all significantly more frequent in the patient group than in the control group. Most of the patients (75%) reported a strong association between head neck movements in the atlanto-occipital and atlanto-axial joints and triggered attacks of vertigo. Also, 29% of the patients could influence their tinnitus by mandibular movements. Signs of cervical spine disorders, such as limitations in side-bending and rotation movements, were significantly more frequent in the patient group than in the control group. Tenderness to palpation of the transverse processes of the atlas and the axis, the upper and middle trapezius, and the levator scapulae muscle were also significantly more frequent in the patient group. The study shows a much higher prevalence of signs and symptoms of cervical spine disorders in patients diagnosed with Meniere's disease compared with control subjects from the general population.
J Orofac Pain. 1996 Winter;10(1):28-37.
Craniomandibular disorders in patients with Menière's disease: a controlled study.
Bjorne A, Agerberg G.
Abstract
This study compares the frequency of signs and symptoms of craniomandibular disorders and dental conditions in patients diagnosed with Menière's disease and in control subjects from a population sample. Thirty-one patients (12 men, 19 women) diagnosed with Menière's disease were referred from three otolaryngologic clinics for clinical examination and possible treatment of craniomandibular disorders. Thirty-one control subjects were selected from the population in the same area of Sweden (Ystad). Both groups were subjected to a screening of their symptoms with a self-administered questionnaire and to a routine stomatognathic examination. The function of the masticatory system was further calculated according to the index of Helkimo for both anamnestic dysfunction (Ai) and clinical dysfunction state (Di). Clinical symptoms of craniomandibular disorders such as pain in the face or jaw; pain on movement of the mandible; fatigue of the jaws; and pain located in the vertex area, the neck/shoulder area, and the temples all occurred significantly more often in the patient group. Findings at the clinical examination included a statistically higher frequency of tenderness to palpation of the masticatory muscles, the temporomandibular joint, and the upper part of the trapezius muscle in the patient group compared to that of the control group. The findings indicate a much higher prevalence of signs and symptoms of craniomandibular disorders in patients diagnosed with Menière's disease than in the general population.
HNO. 1993 Jan;41(1):7-10.
[Correlation between inner ear disorders and temporomandibular joint diseases].
[Article in German]
Kempf HG, Roller R, Mühlbradt L.
Abstract
Acute and chronic inner ear diseases involve many etiological factors, some as yet unknown. ENT-specific, orthopedic, hemorrheological, immunological and neurological disorders can affect the cochleovestibular system and induce hearing loss, vertigo and/ortinnitus. We performed a prospective study to analyze factors of the dentognathological system and of the temporomandibular joint that can influence acute and chronic inner ear dysfunctions. A total of 138 patients (49.3% female, 50.9% male) receiving clinical treatment for inner ear dysfunctions (12.3% chronic sensorineural hearing loss, 15.2% Ménière's disease, 52.2% sudden hearing loss, 13.8% isolated tinnitus, 6.5% recurrent hearing loss) underwent a prospective dental and gnathological examination. In particular, the patient's dental status and a functional investigation of the masticatory muscles and the temporomandibular joint were analyzed. In 20.3% patients the examination showed no pathology of the dentognathological system. In contrast, there were pathological findings in 110 patients (79.7%): in 43.5% a temporomandibular joint syndrome was diagnosed, in 29% parafunction of the occlusion, and in 35% a myopathy of the masticatory muscles. Additionally 32.6% patients showed dental disorders that required treatment; 11.65% had problems with dentures and 20.3% malpositioned wisdom teeth. In 16 patients the recommended dental treatment was followed up and improvement of otological symptoms was found in 56.6%. The present investigation shows that many patients with inner ear dysfunction suffer from dentognathological disorders. For a subgroup of patients there exists the possibility of improving otological symptoms by dental treatment. Therefore we recommend a dentognathological examination in patients with inner ear dysfunctions of unknown etiology.
Int Tinnitus J. 2007;13(2):132-7.
The potential role of joint injury and eustachian tube dysfunction in the genesis of secondary Ménière's disease.
Franz B, Anderson C.
Abstract
Ménière's diseasenot only includes the symptom complex consisting of attacks of vertigo, low-frequency hearing loss, and tinnitus but comprises symptoms related to the eustachian tube, the upper cervical spine, the temporomandibular joints, and the autonomic nervous system. Quantifiable experience shows that the insertion of a middle-ear ventilation tube can alleviate Ménière's disease symptoms, suggesting that eustachian tube dysfunction is a contributing feature. Clinical practice also shows that treating disorders of the upper cervical spine and temporomandibular joints can lessen Ménière's disease symptoms, suggesting a relationship. Similarly, stellate ganglion blocks can be beneficial in controlling Ménière's disease symptoms, highlighting the influence of the autonomic nervous system. Thus, contrasting symptoms associated with the eustachian tube, the upper cervical spine, the temporomandibular joints, and the autonomic nervous system relate to Ménière's disease, but the possible reflex pathway by which a link is established is unclear. We made an attempt in this study to describe a hypothetical reflex pathway that links joint injury and the autonomic nervous system, where eustachian tube function is under their influence and is the critical link. In this hypothetical reflex pathway, irritation of facet joints can first lead to an activated anterior cervical sympathetic system via an independent pathway in the mediolateral cell column; it can simultaneously lead to an axon reflex involving nociceptive neurons, resulting in neurogenic inflammation and the prospect of a eustachian tube dysfunction. The eustachian tube dysfunction is responsible for a disturbed middle ear-inner ear pressure relationship, circumstances that have the potential to develop into secondary Ménière's disease. This reflex pathway is supported by recent animal experiments.
Prog Brain Res. 2007;166:215-9.
Assessment of temporomandibular and cervical spine disorders in tinnitus patients.
Björne A.
Abstract
In treating patients with temporomandibular joint (TMJ) dysfunction it was noticed that tinnitus and vertigo were common in such patients and there was also muscular tension in jaw and neck. During treatment of these patients it was also noted that injection of lidocaine in a jaw muscle (m. pt. lat.) reduced not only their muscular problems but also that the tinnitus was reduced while the local anesthetic was active. Evaluation of 39 patients with disabling tinnitus, and all suffered from tinnitus, revealed that 10 of them had bilateral tinnitus and TMJ disorders revealed that pain in the face, temples or jaw occurred often among these patients. Many of such patients had also symptoms of cervical spine disorders, head, neck and shoulder pain, and limitations in side bending and rotation were also frequent complaints. One-third of these patients could influence tinnitus by jaw movements and 75% could trigger vertigo by head or neck movements. Treatment of jaw and neck disorders in 24 patients with Ménière's disease had a beneficial effect on not only their episodic vertigo but also on their tinnitus and aural fullness. At the 3-year follow-up, intensity of all symptoms were significantly reduced (p<0.001).
International Congress of Craniomandibular Orthopedics Anthology 2016: (accepted and in press)
Two case reports of Meniere’s Disease that responded to computer-guided occlusal therapy
Sutter, B
Abstract
This report reviews two patients diagnosed with Meniere’s Disease that were treated with computer guided occlusal therapy. Each patient was diagnosed with Meniere’s by separate groups of otolaryngologists (ENT). Following a review of medical histories and diagnostic workup evaluation which included CBCT, EMG evaluation, jaw tracking, joint sonography and digital occlusal analysis, it was discovered that there was an underlying dental component that could be corrected. Both patients elected to move forward with treatment of the occlusion in hopes of eliminating their respective symptomology. After the completion of discussion time reduction (DTR), both patients reported significant improvement in their symptoms.